Evaluating care transitional model through the lens of room readiness
With over two months of research (79 hours of observation with 89 hospital staff which covered 10 ancillary departments) with a 26 person team, key insights emerged that helped us identify what the efficiencies and inefficiencies were in the process of getting a room ready to give care to a new admit.
Key gaps in the system that contributed to inefficiencies were: 1) no clear definition of a “ready room” amongst staff, 2) no clear process for getting a room ready (everyone did it their own way), 3) no clear ownership amongst staff of their responsibilities (everyone thought it was someone else’s job), and 4) no way to get critical information on new patient prior their arrival (a wait and see guessing game).
Ideas that were iterated on and tested included: 1) communication method for staff to signal when a room is ready to accept new patient (vs accepting prior a room being ready), 2) a tool for floor managers to capture critical new patient info for assigned RN so they can get mentally and logically prepare to accept new patient (diagnosis, medications, immediate needs, etc.), 3) a checklist tool to identify what equipment is or is not yet in the room, and lastly, 4) pre-packaged hygiene kits (to save time from having to hunt and gather supplies).
Pilot Site Outcomes included: 1) an increase in patient and staff satisfaction scores, 2) an increase in room readiness, 3) an increase in patient throughput efficiency, and 4) an organizational recommendation to adopt all solutions.
Additional outcomes include: 1) Our work being published in various medical journals, 2) the successful completion of the Gordon + Betty Moore grant project “Evaluation of Transitional Care Model within Kaiser Northern California”, and 3) inspiring Allen Cooper and Brian Herriot to co-found “ReadyList” - the premier solution for ensuring fully operational clinical environments, from inpatient rooms and ORs to clinical practices.
-
Kaiser Permanente
Gordon + Betty Moore Foundation
Anita Tucker, Harvard
Role: Research + Design Lead -
#1 - Reduce waste and increase in-patient throughput.
#2 - Increase patient and staff satisfaction scores (by Increasing RN’s time @ bedside).
#3 - Increase patient safety -
Create a way to monitor efficiency and effectiveness of processes that contribute to room readiness.
-
~ 40% increase in room readiness
_ Happier staff and patients
_ Inspiring the creation of ReadyList -

Shadowing staff during research

Understanding current "new patient room" process

Full Team meeting on MedSurg floor

Analogous research: restaurant table readiness process
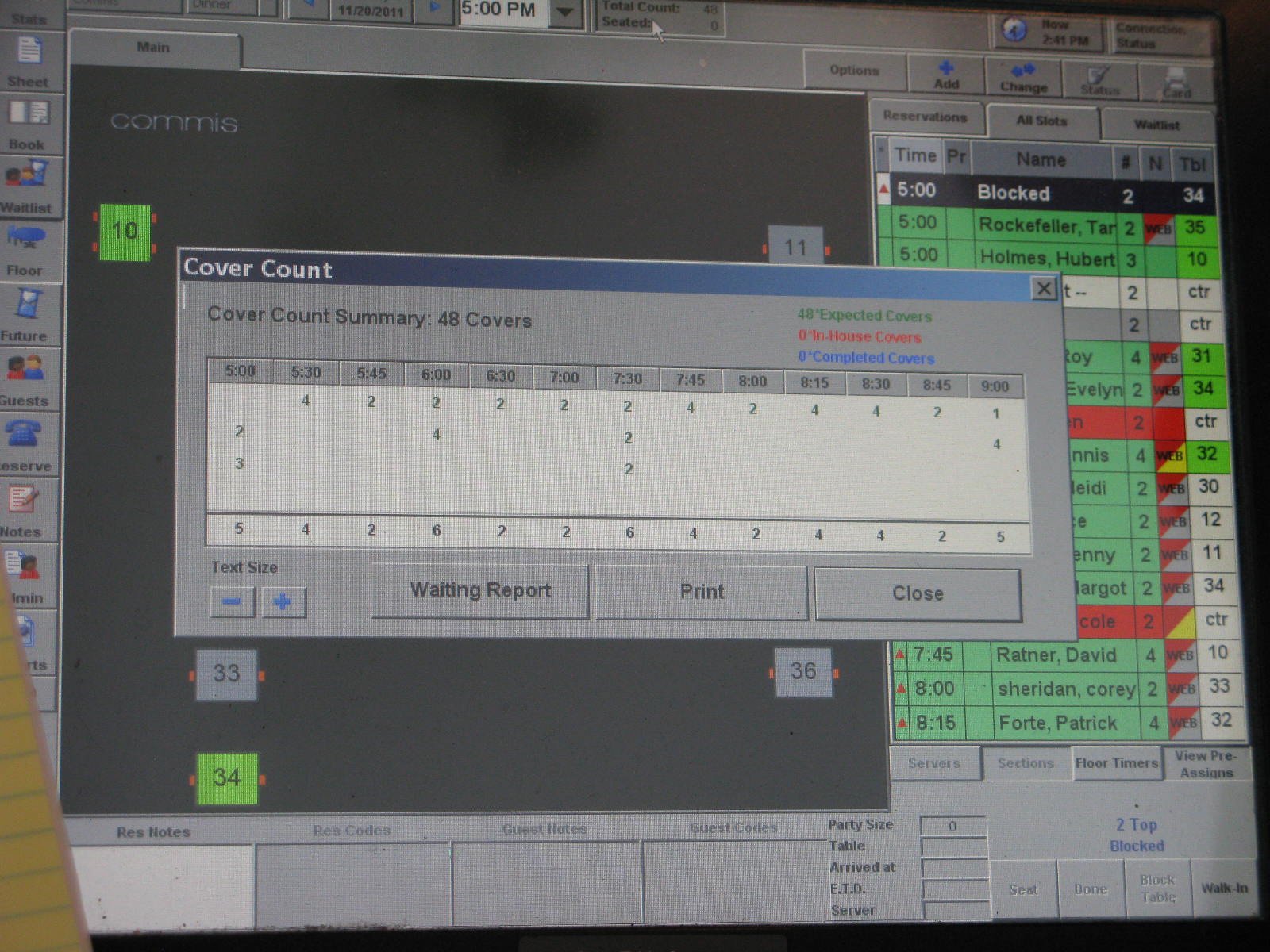
Exploring various efficiency dashboards across various industries

Insight gathering from IT team - what are tools/processes they use to see patient throughput at a hospital system level?

Prototypes: 1) visualizing stages of process, 2) a way to capture new patient info, 3) a way to document what is in vs missing from room, 4) pre-packaged hygiene kits

Metrics showing impact post test of prototype/ideas

Not only does a room need to be ready, but so does the nurse.

Kaiser Permanente Pilot Review
Inspired by this work, ReadList was created.